The routine use of beta-blockers in patients post–myocardial infarction with a preserved LVEF has been a cornerstone of pharmacological treatment protocols. However, the evidence behind their use comes largely from studies performed more than four decades ago, before contemporary reperfusion strategies and modern secondary-prevention therapies were available. Current AHA/ACC guidelines recommend use of beta-blockers in all post-MI patients (Class I), whereas ESC guidelines adopt a more conservative stance, with a Class IIa recommendation for patients with LVEF ≥50%. Until recently, no robust data were available to challenge these practices.
A new meta-analysis of five open-label, superiority RCTs was presented at the AHA Congress in November 2025, accompanied by a simultaneous publication in the New England Journal of Medicine. The analysis examined the role of beta-blockers in post-MI patients with preserved LVEF ≥50%. A total of 17,801 patients were enrolled in the REBOOT, REDUCE-AMI, BETAMI, DANBLOCK and CAPITAL-RCT trials and randomised to beta-blocker therapy (49.6%) or no beta-blocker (50.4%). Median follow-up was 3.6 years. The choice and dose of beta-blocker therapy were clinician-directed in all trials except CAPITAL-RCT, in which all patients received carvedilol. Patients with alternative indications or contraindications for beta-blockers were excluded.
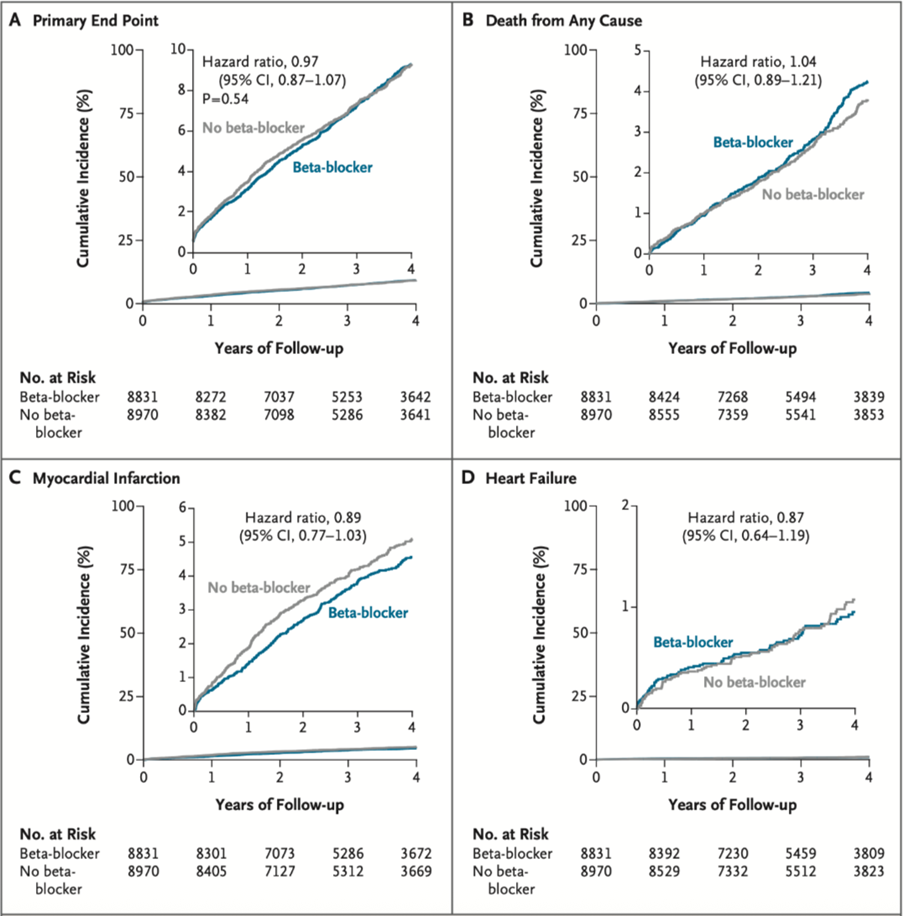
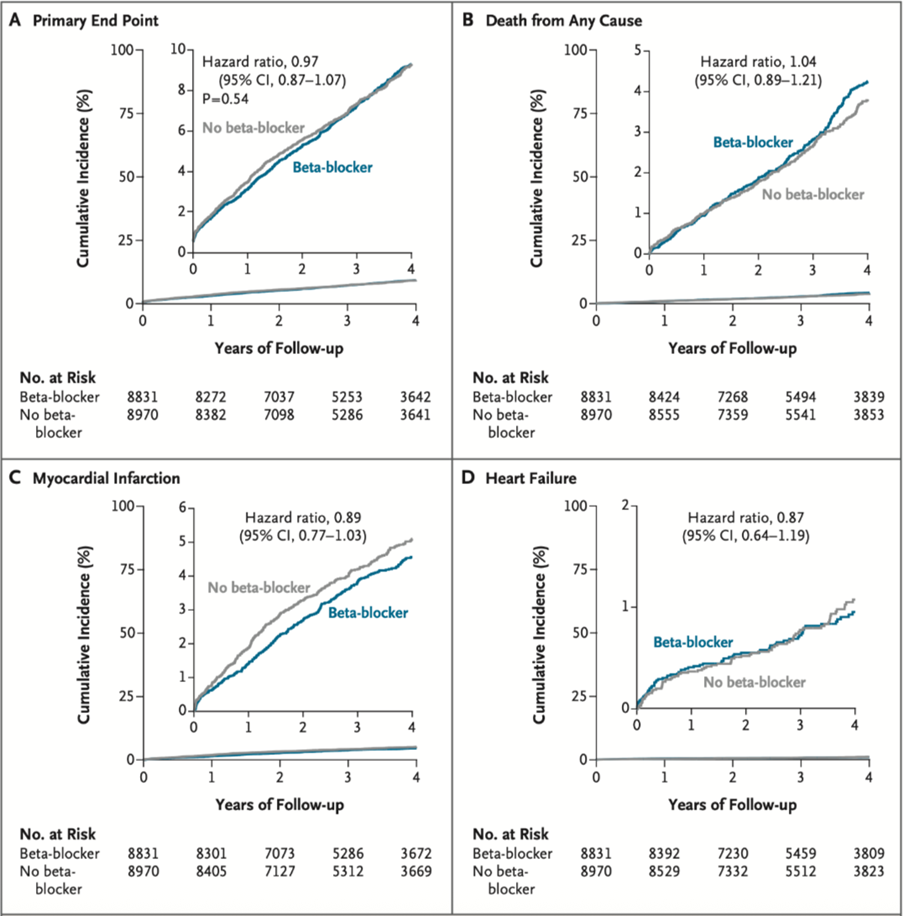
The primary endpoint was a composite of all-cause mortality, myocardial infarction or heart failure. Secondary endpoints included all the individual components of the primary endpoint, as well as cardiac death, unplanned coronary revascularisation and malignant ventricular arrhythmias.
Results
The composite primary endpoint occurred in 335 patients (8.1%) in the beta-blocker group and in 326 patients (8.3%) in the no beta-blocker group (HR 0.97; 95% CI, 0.87–1.07; p=0.54). Across all secondary endpoints, including recurrent MI, HF hospitalisation, cardiac death, revascularisation and ventricular arrhythmias, no significant differences were observed between groups. Rates of ischaemic stroke and high-grade atrioventricular block were also comparable.
Discussion and future directives
Despite the findings recently presented in the BETAMI-DANBLOCK trial, which supported the use of beta-blockers in post-MI patients with EF ≥40%, this meta-analysis demonstrated a consistent lack of benefit in post-MI patients with preserved EF. The neutral effect was highly consistent across prespecified subgroups, including age, sex, Killip class, presence of PCI, baseline heart rate and the specific beta-blocker used.
It is becoming increasingly difficult to support the use of lifelong beta-blockers in all post-MI patients with preserved systolic function, and future guideline revisions are likely to incorporate these new data. However, as highlighted by the noninferiority ABYSS trial, discontinuation of beta-blockers should be carefully individualised, considering patient characteristics, comorbidities and patient preference.
Read the full meta-analysis and individual trials here: https://www.nejm.org/doi/abs/10.1056/NEJMoa2512686 https://www.nejm.org/doi/full/10.1056/NEJMoa2505985 https://www.nejm.org/doi/full/10.1056/NEJMoa2504735 https://www.nejm.org/doi/full/10.1056/NEJMoa2401479 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0199347 https://www.nejm.org/doi/abs/10.1056/NEJMoa2404204